Multiple nurses, docs, an emerita, a pharmacist and spouses from our division on the dance floor shortly after the marriage of Haylee and Sam. Cheers to the newlyweds!

Multiple nurses, docs, an emerita, a pharmacist and spouses from our division on the dance floor shortly after the marriage of Haylee and Sam. Cheers to the newlyweds!

We are proud to announce our division’s contribution to a major clinical study recently published in Diabetes Care: “INHALE-1, A Multicenter Randomized Trial of Inhaled Technosphere Insulin in Children With Type 1 Diabetes.” One of our Division physicians, Dr. Tansey, served as a co-author on this important research. The INHALE-1 trial examined the safety and effectiveness of an inhaled form of insulin compared to standard rapid-acting insulin injections in 230 children and adolescents aged 4 to 17 living with diabetes. Over a 26-week period, participants continued their long-acting basal insulin and used continuous glucose monitoring while receiving either inhaled or injected rapid acting insulin. Compared to the injected insulin group, the inhaled insulin group experienced a similar hemoglobin A1c, similar continuous glucose monitor readings, and lung function. Children using TI reported greater treatment satisfaction and experienced less weight gain compared to those on injected insulin. These findings suggest that inhaled insulin could become a valuable option for some pediatric patients. It is important to note that the study did not compare inhaled insulin to insulin pump-based therapy. The manuscript abstract is available on Pubmed. We especially wish to thank the research coordinators, research participants and their families who made this study possible.
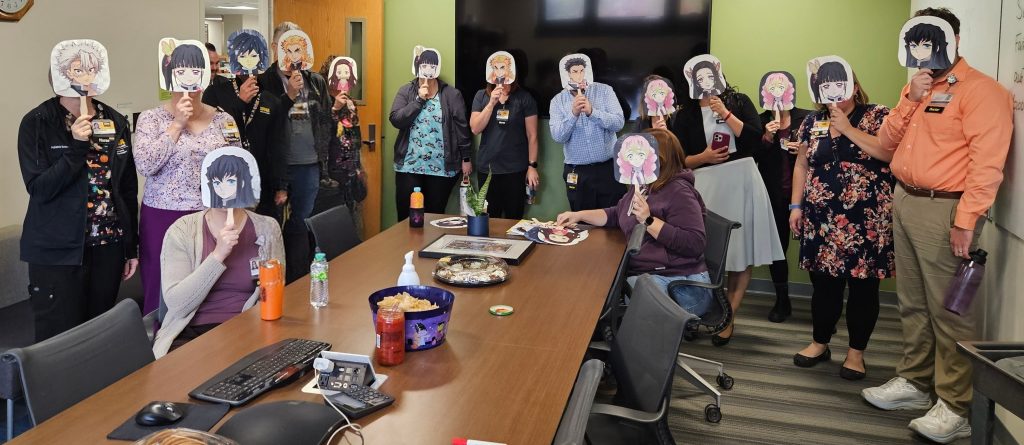
We celebrated the retirement of Rich, endocrinology nurse. We have blessed for over a decade by Rich’s excellence and deep clinical experience, not to mention his collection of weekly humorous memes. Today, we had a luncheon in his honor, complete with anime masks. We wish him a rich journey in retirement.


Multiple division members attended the 2025 fund raising Gala for Breakthrough T1D in Cedar Rapids on November 1st. Breakthrough T1D is the leading non-profit fund raising organization aiming to drive research that finds cures for type 1 diabetes.

At the Gala: Pediatric Diabetes Nurses ready to help with the challenges of T1D!!!

Breakthrough T1D Promise Gala: some of the division attendees and friends!!!

We are excited to share that our Division has been rated among the Best Children’s Hospitals for Diabetes & Endocrinology Care by the US News 2025-2026 annual national report, where we were ranked #33 nationwide. Other top ranked specialties at the University of Iowa Stead Family Children’s Hospital included neonatology (#19), nephrology, urology, pediatric cancer, and behavioral health.
“Our ongoing strong national ranking is a testament to the steadfast dedication and expertise of our pediatric endocrine physicians, nurse practitioners, specialty nurses, diabetes educators, psychologists, researchers, medical assistants, dieticians, pharmacists, social workers, and all teams members. We remain devoted to provide the best endocrine and diabetes care for the children and adolescents in the region and beyond.”
Andrew Norris, M.D. Ph.D.
Director, Division of Endocrinology and Diabetes
UI Stead Family Children’s Hospital

Lifestyle interventions can be a very powerful means to impact adolescent obesity. However lifestyle counseling of adolescence is notoriously difficult. Physicians are often poorly trained to meet this challenge. These discussions are fraught with some risk that insensitive approaches might trigger disordered eating and/or disturbed body image. To help physicians address these challenges, Dr. Lauren Kanner from our division is part of a team delivering a lecture entitled “Neither Feast nor Famine: Weight-Inclusive Approaches to Counseling Youth with Higher BMIs”. This lecture aims to provide physicians with strategies to effectively counsel adolescents to enact positive lifestyle changes. The lecture will be delivered by Dr. Kanner in conjunction with Dr. Maya Kumar from Rady Children’s Hospital. The lecture is co-sponsored by Society for Adolescent Health and Medicine (SAHM) and the North American Society for Pediatric & Adolescent Gynecology (NASPAG). The webinar will occur on October 8, 2025. See this link to sign up to view the webinar.
On September 19th, Dr. Ramakrishna from our division co-presented Pediatric Grand Rounds along with pediatric psychologist Dr. Laura Fuller. Their talk, entitled “Treating Patients with Differences of Sexual Development: The Intersection of Medicine and Psychology”, explored the complexities of the medical and psychological healthcare of Differences of Sexual Development (DSD).
DSDs encompass a group of conditions in which the typical processes of sexual development—anatomical, hormonal, functional, and reproductive—do not follow the usual male or female patterns. These variations may be apparent at birth or even prenatally, though some forms may not be diagnosed until adolescence or adulthood.
The primary goal of pediatric DSD care is to support the physical and emotional well-being of affected individuals during youth. During their presentation, Drs. Ramakrishna and Fuller provided an overview of the various types of DSDs and illustrated the unique medical and psychosocial needs of patients through case examples. They emphasized the importance of a multidisciplinary approach to care.
Drs. Ramakrishna and Fuller lead a multidisplinary DSD clinic that includes pediatric endocrinologists, pediatric urologists, clinical geneticists, and pediatric radiologists, with support from reproductive endocrinology and clinical pharmacy services.
We extend our sincere thanks to Drs. Ramakrishna and Fuller for their insightful presentation and for their leadership in delivering expert, compassionate DSD care through their multidisciplinary team.
On September 23, Dr. Alexandrou from our division will be helping present psychiatry grand rounds on the topic of “mental health care/screening in Turner’s syndrome“. Dr. Alexandrou will have a co-speaker on the topic, Dr. Erin Olufs, who is a child psychologist. They will be speaking about the importance of screening for mental health issues in youth and young adults with Turner syndrome. Research has shown that women with Turner syndrome have increased risk of a variety of mental health concerns, including anxiety, depression, and autism spectrum disorders among others. Screening for these conditions is important and early and skilled intervention can be helpful. We are grateful that Drs. Alexandrou and Olufs will be able to share their expertise and experience in this important area of health care.