type 1 diabetes inpatient management
 Post by
Post by
Andrew Norris, MD PhD
Director, Pediatric Endocrinology & Diabetes
University of Iowa Stead Family Children’s Hospital
“it is incumbent upon the pilot/physician to keep ‘one hand on the throttle and one on the stick’ by providing both glucose and insulin when someone with type 1 diabetes is unable to eat…“
Managing type 1 diabetes is challenging, including for physicians. Often a physician naturally feels caught between two opposing fears.
- Fear #1: “if too much glucose is given, the blood sugar might go too high”
- Fear #2: “worse yet, if too much insulin is given then the blood sugar can go dangerously low”
These fears are real and represent real risks. The fear of these is especially heightened when managing diabetes in someone who is unable to eat. Unfortunately, these two fears present a false dichotomy that can lead to a cognitive error. The specific error logic is as follows:
- Response to fear #1: “if glucose is not given, then the blood sugar can’t go high“
- Response to fear #2: “if insulin is not given, then the blood sugar can’t go low“
The physician then writes orders that omit glucose (i.e. dextrose) from the IV fluids and under-dose insulin. Although this approach at first seems like a reasonable way to resolve the above conundrum, it can lead to serious issues. A useful analogy is that this is similar to flying a plane by cutting power to the engine and taking one’s hands off the stick. To better understand this, let’s first explore what happens when someone without diabetes is not given any glucose or carbs as they undergo fasting. The figure immediately below shows what happens to their plasma glucose, insulin and ketones levels.
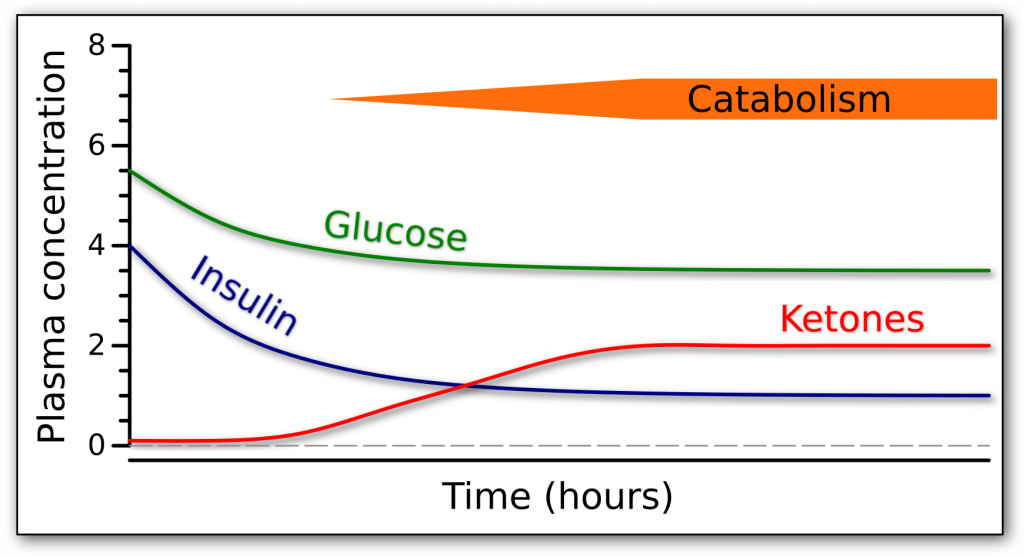
As shown in the figure, during fasting, glucose levels drop as expected, and in response insulin levels drop . But importantly, insulin levels do not drop to zero, but rather decline to a low but basal level. As insulin levels become low, this induces a catabolic state including the production of ketones. Key to this process is the fact that a low level of insulin remains to keep ketone production in check. To use our simplistic analogy, even though we let go of the airplane controls, autopilot has kicked in, courtesy of the beta-cells that maintain a basal degree of insulin secretion.
Let’s contrast this to what happens in someone with type 1 diabetes who can not make their own insulin. In this case, if insulin is not being given, levels eventually fall to zero, as shown in the next figure.
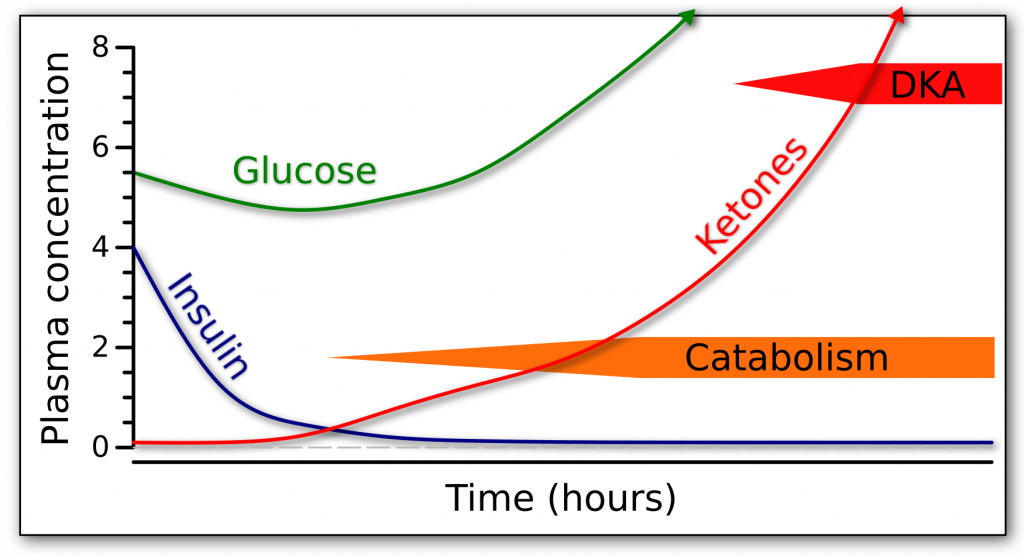
When insulin levels become abnormally low, two important things happen. Firstly, this triggers runaway gluconeogenesis, eventually leading to formation of new glucose and onset of spontaneous hyperglycemia. In other words, even though the person is not receiving glucose, their blood sugars rise because of the production of new glucose by their liver. Secondly, the abnormally low insulin levels allow runaway ketone production, eventually leading to diabetic ketoacidosis. To return to our simplistic analogy, our airplane has crashed and burned. When insulin levels reach zero, our engine can no longer burn fuel properly (i.e. insulin enables cells to properly utilize glucose), and gravity (i.e. run-away catabolism and ketone formation) ultimately wins.
Often, and typically in pediatrics, glucose is provided intravenously to patients without diabetes who can not otherwise obtain nutrition. It is informative to examine what happens to plasma insulin, glucose, and ketones in this situation, as shown in the next figure.
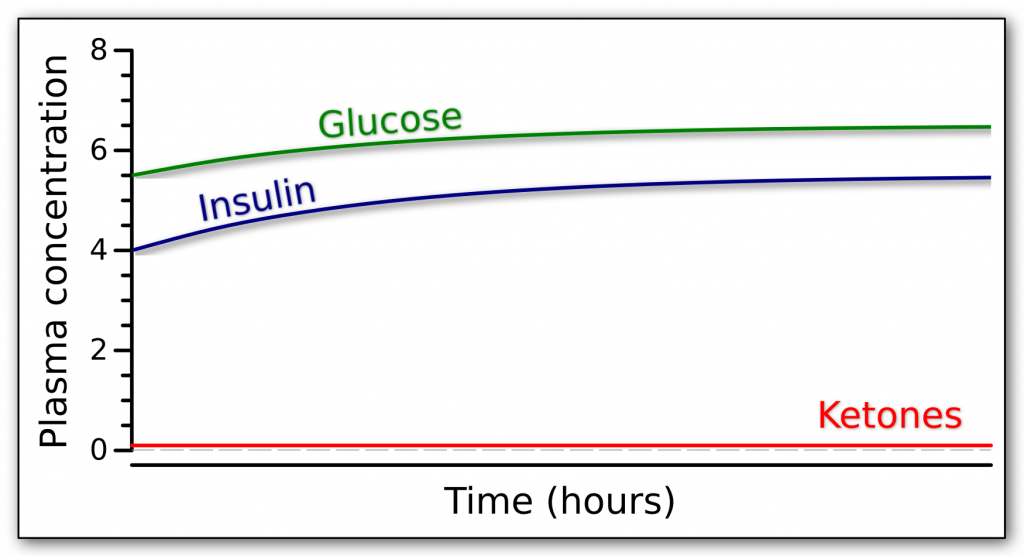
As is shown in the figure, the ongoing administration of intravenous glucose causes blood sugar to rise some, but the body responds by increasing insulin to compensate such that blood sugar remains normal. Importantly, because insulin does not reach low levels, ketone production remains suppressed and catabolism is avoided. This is a safe state for the patient. To keep a patient with diabetes safe, the physician can mimic this state by providing insulin and glucose. The insulin and glucose must be counterbalanced, and importantly insulin levels must be maintained always at a basal level, either through provision of long acting insulin or via intravenous insulin drip. Additionally , the blood sugars typically will vary. Despite this, because insulin is being continually supplied, ketone production is suppressed and the patient remains safe. The next figure illustrates this approach.
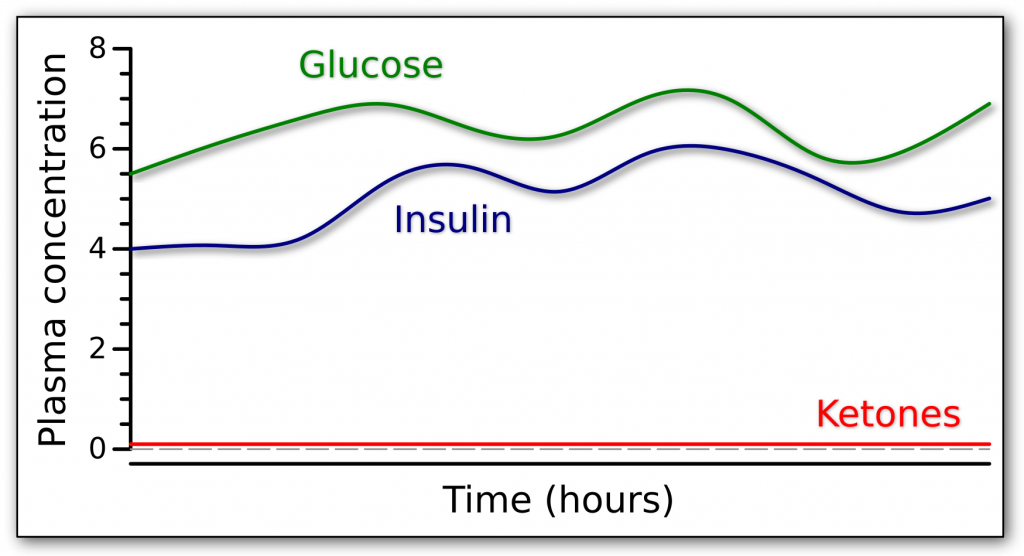
Although the blood sugar varies, the patient remains safe because insulin levels do not fall to zero and because glucose is administered to maintain blood sugar levels. This way run-away catabolism and ketone formation are avoided, as are hypoglycemia and severe hyperglycemia.
Returning to our airplane analogy, functioning beta-cells are our usual autopilot. Someone with normally functioning beta-cells can be fasted or fed or given IV dextrose and remain euglycemic, avoiding hypoglycemia and ketoacidosis. In type 1 diabetes this autopilot is absent and it is incumbent upon the pilot to keep one hand on the throttle and one on the stick. Just like flying a plane, with study, practice and experience, the flight can be less turbulent.
In infants, children and adolescents with type 1 diabetes, the risks are heightened. Infants and children develop ketones at a more rapid pace than adults, and adolescence induces a state of physiological insulin resistance. Likewise, during illness and medical stress, the drive towards catabolism is increased, and the risks of crashing greater. Please know that your local pediatric endocrinology team remains happy to assist, helping ensure many safe landings.
Some notes: (1) Although the above discussion is simplified in many ways and the actual involved physiology is complex, nonetheless almost without exception out-of-control ketogenesis ensues when insulin levels become extremely low. (2) In the airplane analogy, gravity represents the incessant pull towards catabolism when insulin levels are low. (3) Although we think of dextrose containing fluids as driving major hyperglycemia, it should be remembered that 100 mL of D5 contains only 5 grams of glucose, about the same as 3 skittles or 2 saltine crackers. Interestingly, hepatic glucose production during routine fasting (i.e. overnight) is roughly the same as D10 containing IV fluids running at maintenance rates. For this reason, many metabolism experts advocate D10 containing IV fluids at maintenance rates to best avoid catabolism in patients both with and without diabetes. (4) Please know that blood glucose and plasma glucose are nearly equivalent, especially conceptually for the above purpose, and are thus used interchangeably above. (5) I don’t have actual data that this is the most common severe conceptual error in managing inpatient diabetes, but rather this reflects over a decades experience. (6) On a brief personal note, I would like to thank my life partner for proofing this.

