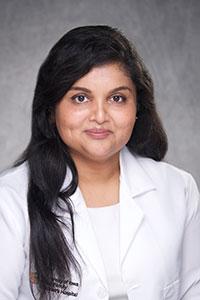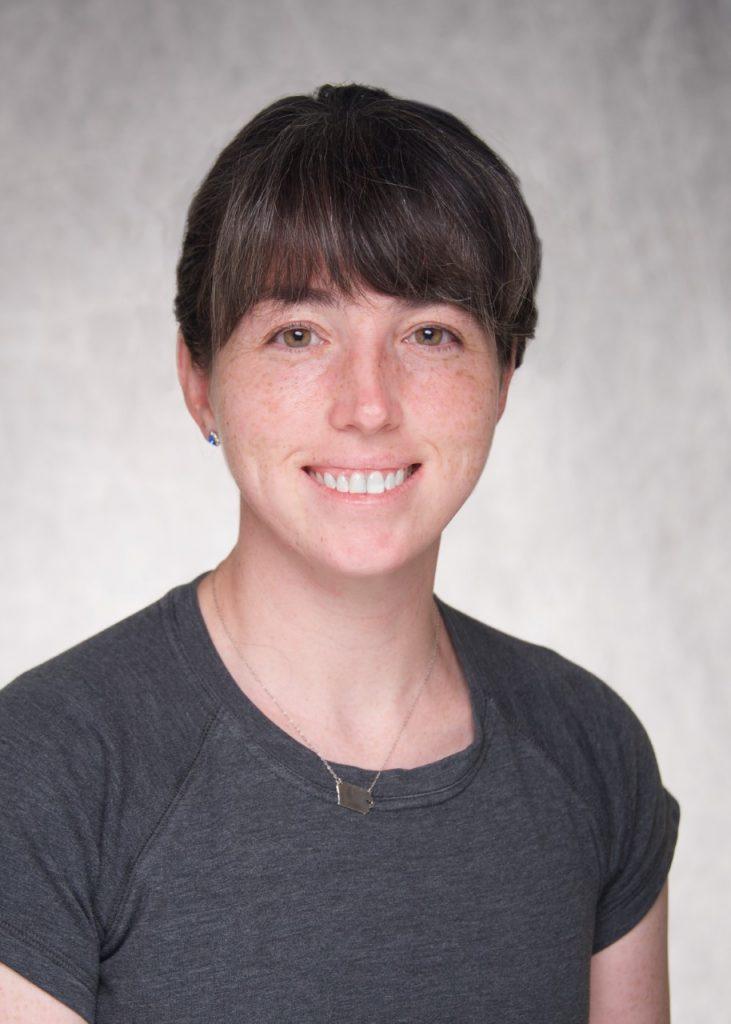
A variety of pathological processes can induce puberty earlier than otherwise would normally occur. When a child enters puberty, an important question is whether the timing is abnormally early. Pediatric endocrinologists are often the arbitrators of this question. Data defining the normal ages of puberty start are thus important. Data suggest that normal timing varies depending on a child’s genetics and environment. A recent publication in JAMA Network Open reports data collected from over 100,000 youth with Asian American, Native Hawaiian, and/or Pacific Islander heritage (link to article). To help interpret the findings, Drs. Vanessa Curtis and Catherina Pinnaro from our division were asked to provide their commentary on the article. Their commentary can be found here (link, which has link to the open source full text). They conclude that “[the] study […] emphasizes the necessity for precision and the pitfalls encountered when using race and ethnicity as a proxy for genetic background.”