Dr. Tansey 
Dr. Tsalikian
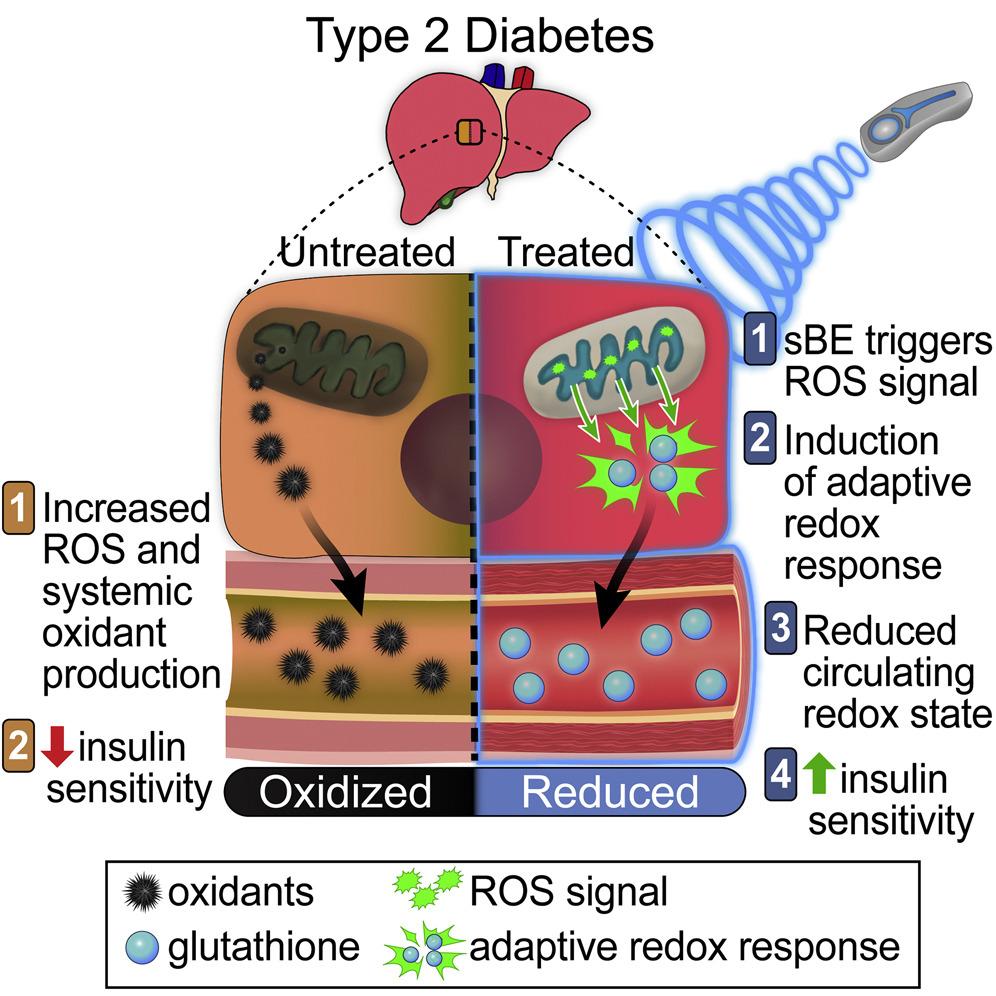
It has previously been observed that young children with type 1 diabetes have changes in brain structure, when compared to children without diabetes. However, it has not been known how these differences in brain structure might change over time. To help address this knowledge gap, Drs. Tsalikian and Tansey have helped conduct a multicenter longitudinal trial following over 100 children with type 1 diabetes. The children underwent repeated brain imaging with MRI over an average span of 6 years time. The results from this study have now been published in the prestigious journal Diabetes Care (link). The study found that the brains of children with type 1 diabetes exhibited smaller volume, and that this difference became greater over time. Importantly, higher blood sugar levels were correlated with greater loss of brain volume. These results lend further credence to the notion that loss of brain tissue is a complication of childhood diabetic hyperglycemia. Furthermore, the results suggest that meticulous glycemic control might prevent these structural brain changes. Since the study was correlative, these conclusions are not fully definitive and further study is needed. It remains crucial that children with diabetes be followed by an expert pediatric endocrinology team, such as at the University of Iowa. Several other of our division members contributed to this work, including study coordinators Julie Coffey MSN and Rachel Bisbee. We also thank the families and children who volunteered as participants in this study.